Evidence-Based Lower Limb Assessments for Strength, Endurance, and Functional Capacity
Jan 16, 2026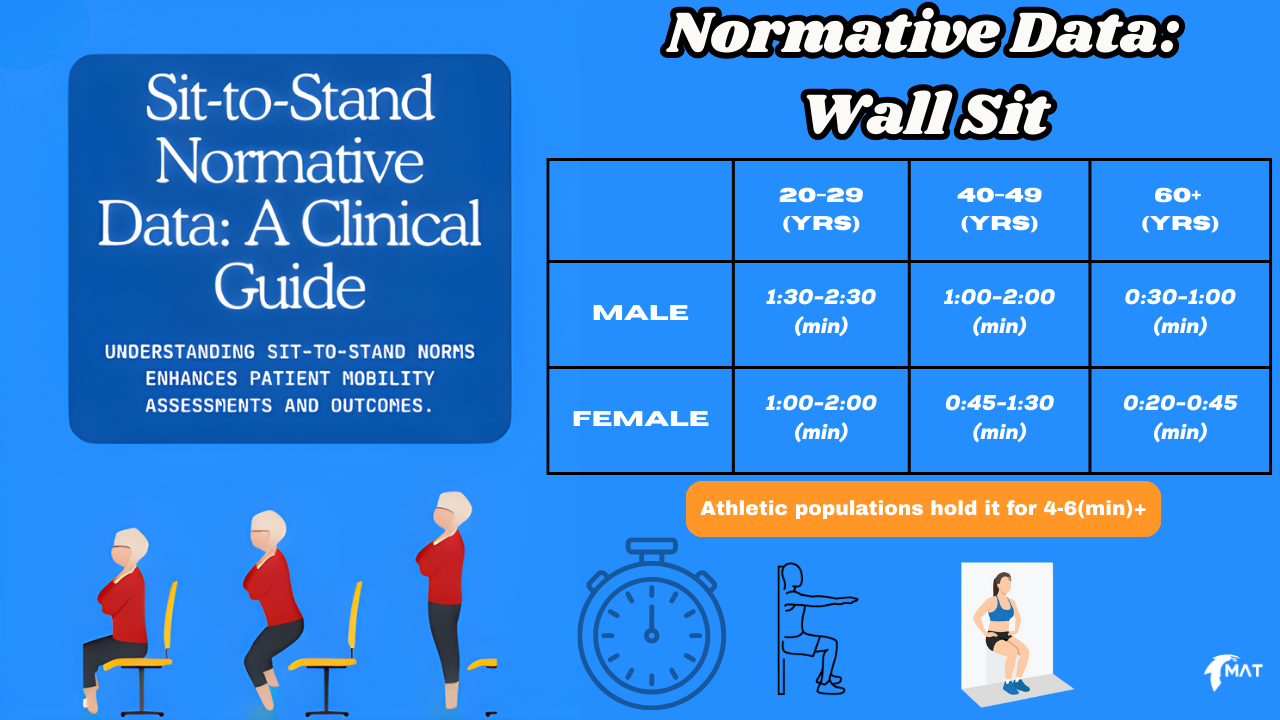
Lower-limb function underpins independence, work capacity, and athletic performance. While isolated strength tests provide useful data, they often fail to reflect real-world movement demands.
Two of the most validated, time-efficient, and underused assessments in lower-body evaluation are:
-
The Sit-to-Stand (STS) Test
-
The Wall Sit Test
Despite their simplicity, both tests provide clinically meaningful insight into strength, power, endurance, motor control, and functional capacity across a wide range of populations.
Why Assess Sit-to-Stand and Wall Sit Performance?
Key Benefits of These Tests
-
Functional and task-specific
-
Easy to standardise
-
Minimal equipment required
-
Sensitive to change over time
-
Strongly associated with real-world outcomes
Importantly, both tests assess capacity under load, which is more relevant than isolated muscle output alone.
Sit-to-Stand Test (STS)
What Does the Sit-to-Stand Test Measure?
The STS test reflects a combination of:
-
Quadriceps and gluteal strength
-
Functional lower-limb power
-
Balance and postural control
-
Movement efficiency
-
Fatigue tolerance
-
Cardiovascular contribution (particularly in repeated protocols)
Standing from a seated position is a universal task, making STS performance highly transferable to daily living, work tasks, and sport-specific demands.
Sit-to-Stand Test Protocols
5× Sit-to-Stand Test (5xSTS)
Purpose: Emphasises strength and power
Standardised Setup
-
Chair height: 43–45 cm
-
Arms crossed over chest
-
Back against chair at start
-
Feet flat and consistent placement
Procedure
-
On “go,” stand fully upright
-
Sit fully back down
-
Complete five repetitions as fast as possible
-
Record total time
-
Observe compensations
-
Repeat if reliability is required
30-Second Sit-to-Stand Test (30s STS)
Purpose: Emphasises muscular and cardiovascular endurance
Procedure
-
Same setup as 5xSTS
-
Perform as many full repetitions as possible in 30 seconds
-
Count only complete repetitions
-
Observe quality as fatigue develops
Normative Sit-to-Stand Data (General Guide)
5xSTS (seconds)
-
< 11 sec: Above average
-
11–14 sec: Typical range
-
14 sec: Reduced capacity
-
16 sec (older adults): Increased fall risk
30s STS (repetitions)
-
Young adults: ~20–25+
-
Middle-aged adults: ~14–20
-
Adults 60–69:
-
Men: ~14–19
-
Women: ~12–17
-
-
< 12 reps: Reduced functional strength
Normative values provide context, not diagnosis. Longitudinal change is often more informative.
What to Observe Beyond the Score
Quantitative results should be interpreted alongside movement quality, including:
-
Knee valgus or medial collapse
-
Excessive trunk momentum
-
Uneven limb loading
-
Poor eccentric control
-
Loss of rhythm or pacing
-
Use of hands
These patterns often indicate strength asymmetry, control deficits, or fatigue intolerance.
Wall Sit Test
What Does the Wall Sit Test Measure?
The wall sit is an isometric assessment primarily reflecting:
-
Quadriceps endurance
-
Isometric strength capacity
-
Knee and hip load tolerance
-
Neuromuscular control under sustained demand
Because movement is removed, the test isolates endurance and fatigue resistance more effectively than dynamic tasks.
Wall Sit Normative Benchmarks
General Population – Men
-
20–29 yrs: ~90–150 sec
-
40–49 yrs: ~60–120 sec
-
60+ yrs: ~30–60 sec
General Population – Women
-
20–29 yrs: ~60–120 sec
-
40–49 yrs: ~45–90 sec
-
60+ yrs: ~20–45 sec
Athletic populations often exceed 4–6 minutes, particularly in sports with high isometric demands.
Technical Standards and Common Breakdowns
Correct Position
-
Thighs ~parallel to floor
-
Knees ~90° over ankles
-
Back against wall
-
No hand support
Common Compensations
-
Knees drifting forward
-
Hips rising or collapsing
-
Asymmetrical shaking
-
Early unilateral fatigue
These breakdowns often appear before task failure, providing valuable diagnostic information.
Clinical and Practical Relevance
General Population
-
Functional independence
-
Stair and transfer ability
-
Daily task tolerance
Older Adults
-
Fall risk prediction
-
Preservation of lower-limb strength
-
Activities of daily living (ADL) capacity
Athletic and Active Populations
-
Strength vs endurance discrepancies
-
Fatigue tolerance under load
-
Limb asymmetries not evident in maximal testing
Why Use Both Tests Together?
The Sit-to-Stand test reflects dynamic functional performance, while the wall sit isolates isometric endurance.
Together, they provide a more complete picture of lower-limb capacity than either test alone.
Key Takeaway
Simple assessments can still be powerful.
The Sit-to-Stand and Wall Sit tests are among the most efficient, evidence-supported, and transferable tools for evaluating lower-limb strength, endurance, and functional capacity. When used consistently, they support clearer baselines, better progress tracking, and more confident decision-making.
FAQ
❓ What does the sit-to-stand test assess?
The sit-to-stand test assesses lower-limb strength, functional power, balance, endurance, and movement efficiency during a real-world task.
❓ How long should you be able to wall sit?
Wall sit duration varies by age and sex. Most adults can hold between 30–150 seconds, while trained athletes often exceed 4 minutes.
❓ Is the sit-to-stand test reliable?
Yes. Multiple studies demonstrate high test–retest reliability and strong associations with functional outcomes and fall risk.
References
Alcazar, J., Losa-Reyna, J., Rodriguez-Lopez, C., et al. (2018).
The sit-to-stand muscle power test: An easy, inexpensive and portable procedure to assess muscle power in older people.
Experimental Gerontology, 112, 38–43.
https://doi.org/10.1016/j.exger.2018.09.007
Barry, E., Galvin, R., Keogh, C., Horgan, F., & Fahey, T. (2014).
Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: A systematic review and meta-analysis.
BMC Geriatrics, 14, 14.
https://doi.org/10.1186/1471-2318-14-14
Bohannon, R. W., & Crouch, R. (2019).
1-minute sit-to-stand test: Systematic review of procedures, performance, and clinimetric properties.
Journal of Cardiopulmonary Rehabilitation and Prevention, 39(1), 2–8.
https://doi.org/10.1097/HCR.0000000000000336
Guralnik, J. M., Simonsick, E. M., Ferrucci, L., et al. (2016).
Physical performance measures in aging research.
The Journals of Gerontology: Series A, Medical Sciences, 71(6), 747–753.
https://doi.org/10.1093/gerona/glw024
Larsson, L., Degens, H., Li, M., et al. (2019).
Skeletal muscle fatigue and ageing.
Physiological Reviews, 99(1), 427–511.
https://doi.org/10.1152/physrev.00020.2018
Orssatto, L. B. R., de la Rocha Freitas, C., Shield, A. J., & Trajano, G. S. (2020).
Lower-limb muscle power, strength and functional performance in older adults.
European Journal of Applied Physiology, 120, 271–283.
https://doi.org/10.1007/s00421-019-04243-0
Reynders, T., Delecluse, C., & Verschueren, S. M. (2019).
Age-related changes in muscle power and functional performance.
Sports Medicine, 49(4), 545–556.
https://doi.org/10.1007/s40279-019-01049-3
Strassmann, A., Steurer-Stey, C., Lana, K. D., et al. (2013).
Population-based reference values for the 1-minute sit-to-stand test.
International Journal of Public Health, 58, 949–953.
https://doi.org/10.1007/s00038-013-0504-z
Treacy, D., & Hassett, L. (2018).
The short physical performance battery.
Journal of Physiotherapy, 64(1), 61.
https://doi.org/10.1016/j.jphys.2017.11.003
Download Our Measurz App For FREE And Perform, Record and Track 800+ Tests With Your Clients Today.
Want To Improve Your Assessment?
Not Sure If The MAT Data-Driven Approach Is Right For You?
Get a taste of our MAT Course and data-driven approach using the MAT with a FREE module from our online MAT Course.
We hate SPAM. We will never sell your information, for any reason.



